This post has been swimming for months now. In all honesty, I have been hesitant to put it out there for a number of reasons. One is that for myself, I really had to process all of what went on, and two, it is not a post that I wanted to write while I was angry. While I want to be honest and real about what went on, I also want to respect the doctors we worked with and the work that they did while we were in hospital. I’ve had a number of people asking about what happened, why we ended up transferring Leevi and how we suddenly ended up at home, but it is also a story that I want to tell and as hard as it was, it is one that I want to remember. I want parents to know that they have a voice, that it’s okay to question things and that your baby needs you to stand up for them… even when you are faced with a circumstance that is so foreign.
If you follow me on social media you will know that Leevi was in the neonatal unit for the first two weeks of his life. If you haven’t already, you can read about his birth here. It was undoubtedly the most difficult two weeks of my life and Phil will say the same. I have never felt so helpless, so uncertain and so emotional EVER.

Leevi was on antibiotics for suspected congenital pneumonia for a a total of 5 days. His CPAP came off on day 3, after 7 days all of his IV’s came out and he was moved to High Care B. But his feeding tube remained. High Care B is the final stop before going home and is referred to by many parents as the departure lounge. It is a bittersweet place to stop – you are so close to going home but there is no end in sight, no timeline is given and every day I found myself gazing longingly at the lucky set of parents who were walking through those doors with their carseat in hand. It is also the unit where the staff are the most relaxed – I wish I could say this is a good thing… for us it wasn’t.
Being a nicu mama is hard on so many levels. It’s hard to have to ask permission to hold your baby, it’s hard to have to leave them while they are lying in an incubator wide awake, it’s hard to see them hooked up to all of those machines, to see that their drip was changed while you were away and to know that you weren’t there to comfort them when it happened, it’s hard to have everybody question your decision to lodge at the hospital and to be the talk of the unit because you sat with your baby until 2am that morning. I was told that I was spoiling my baby numerous times because I rocked him to sleep, I was questioned for doing skin on skin because he was a big baby!?! I was told I would struggle when I took him home because I was ‘spoiling’ him. I was told I needed antidepressants because I was crying a little more than they’d like me to (I do believe that there is a time and a place for them but my problem is that the doctor in question never took the time to get to know me or what I was feeling before making those presumptions). It was utterly exhausting and left me feeling like I was going against the unit on so many different levels.
As we entered our second week in the NNU, we began to question their methods. While Leevi was technically better, he was not drinking at all (all milk feeds were given via his nasogastric tube). We were not allowed to breastfeed (it was believed that this would place too much strain on his heart) and he was not interested in his bottles. Feeds ended with both of us in tears and while I believe the nurses did have our best interests at heart, Leevi’s case was sorely overlooked as they continued to force feed him his bottles (manipulating his chin to mimic sucking) and then feed whatever was not taken via the bottle after 30 minutes through his tube.

We were patient, we believed they knew what they doing and we had confidence in the fact that they were labelled as one of the best nicu’s in the country. After days of what felt like terrific failure and requests to bring in outside help we eventually managed to get an amazing speech therapist in to work with us. In my opinion, they should have called her in the day that Leevi began suck feeds, the day that he didn’t suck for the very first time – why they waited for us to question things before making this call is beyond me. Andrea changed our feeding method completely and we finally started to see some sort of progress. I had gained a little bit of control over his feeds and little by little, our gorgeous guy began to suck. The idea of going home was slowly becoming a little bit of a reality.
If you are familiar with ‘paced feeding’, you will know that it is a very specific method of bottle feeding and for this reason we had requested that I do all bottle feeds (at this point Leevi was having 1 bottle and then 2 tube feeds in a cycle – whatever wasn’t finished during a bottle feed was then fed via tube). Much like breastfeeding, paced feeding allows the baby to lead the feed and so Leevi’s feeds became a lot less stressful, completely unforced and he responded to the method beautifully. He had to finish at least 60ml of each bottle for 3 days before they would move him onto the next cycle and eventually get him onto all bottles before being able to go home. So while things were improving, at this point we were looking at another 10 – 14 days in the neonatal unit.

My heart was constantly torn between being at the hospital with Leevi and being at home with our girls. My days were long ,busy and even amongst everything that had to be done, often lonely. I watched countless moms come into the maternity ward, have their babies and go home again. I mourned for the experience that we had lost and longed to take our baby home. I cried out to God for a miracle, for peace, for courage and for my baby to drink.
Just when we felt like we were gaining a little bit of ground, something else would fall. I was pumping twice the volume of milk that Leevi was ‘drinking’ and twice I found formula next to his crib (I chose to forget about the many times it might have happened but I wasn’t there to witness or correct it). It may sound like a small and insignificant thing to many, but for any nicu mama it is just not on. I was working around the clock to get that milk to him and because the milk kitchen had neglected to read his chart properly, they were simply not preparing enough milk for him to get through the day. I find this completely unacceptable when you are dealing with the most vulnerable patients in the hospital, the ones who cannot speak up for themselves and who really don’t know any different. The final straw for us (after many meetings and questions) was when I went up to see Leevi one Wednesday night. It was a little after 9pm, Phil and the girls had just left for the evening and I had decided that I would quickly pump before going to see Leevi. His 9pm feed was a tube feed which they would often just let the babies sleep through as it didn’t make any difference to them. We had just had a great session with our speech therapist for the earlier feed and we were actually feeling quite encouraged. When I got to his crib I saw an empty bottle standing next to his bed which was strange as according to their method and the feeding schedule he was on, he was not allowed to have one bottle after another. The other thing is that we had specifically asked that I give all bottle feeds due to the method we were now using and the fact that none of the nurses were familiar with paced feeding (I was lodging there after all and I was fully available for feeds). Again, perhaps this seems like a trivial issue, but man, when you are working that hard at getting your baby home and when you have lost all confidence in the manner in which they are being treated, it is huge. By this stage we had spoken to a couple of experts and began to realise that there are many different methods of treating these little people and that this particular one did not in any way seem like the best.
While we do believe that the doctors cared, we think they could have done a better job at communicating with, managing and making use of their team. While they believe that their age old method is the best, we feel it could be better. While we don’t think the nurses were trying to mess up, we feel that they need to pay more attention to each baby and their treatment plan, we believe that their training could be far more specialised and we can only hope that as a team they will learn from what transpired. We also feel that parents could and should be far more involved in the process, we have learnt enough to know that other NICU’s have got this right and I feel that it can only benefit both the family and the baby. We are so grateful for what the doctors did for Leevi and for the quick and effective treatment he got, we just wish it could have ended differently.
After spending that night holding my baby in the breastfeeding room, after many discussions, help from others, much prayer and countless tears, we made the very difficult decision to transfer Leevi to a different hospital where he would be under the care of our family paediatrician. A man that we have worked with and trusted for years, a man who also had a very different approach to Leevi’s situation.
At 20:43pm on Thursday 21 September Leevi was loaded into an ambulance and began his journey home. I cannot tell you how amazing the paramedics were during our transfer – they were a breath of fresh air and made a hectic end to what was a very difficult day so much better. We arrived at our destination just after 9pm where our paed was ready and waiting. After checking Leevi’s vitals he removed his feeding tube and told me to breastfeed my baby. Leevi was two weeks old, he had never even set eyes on a breast before and he could barely suck from a bottle but this little guy latched and drank for 30 minutes without a single issue. I cried so hard as I gazed down at him, taking in his amazing tubeless little face for the first time – he was so perfect and after all that we had been through, he knew that I was his mom.



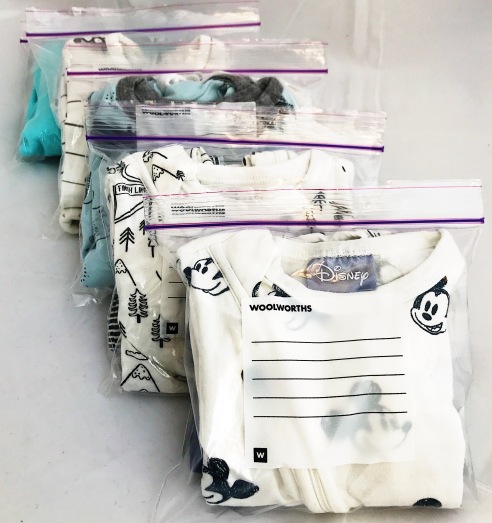
I was sent home that night while he stayed in isolation (standard procedure for babies coming in from other hospitals) which was really good for me. It was good to come home, unpack my bags and ‘reset’. I had no idea how things would play out over the next few days but we had a new sense of energy and a very real kind of hope that we would all be home soon.
When we arrived at the hospital the next morning, Leevi had successfully drank from bottles through the night, he had been bathed and he was ready to be moved into the paediatric ward with me where we were given strict instructions to stay in bed and feed on demand.
This day was such a gift to us. Despite all that we had been through I felt as though Leevi had just been born, as though nothing had ever come between us. He fed beautifully throughout the day and when he wasn’t nursing we were cuddling. We were pretty much left alone to bond for the entire day and when our paed came in to check on us at 5pm he casually told us we could go home. Just like that, at 19:35pm on Friday 22 September 2017 (one day before his due date) we walked out of the hospital with our baby boy safely strapped into his car seat. It was nothing like the homecoming we had imagined and we needed a lot of time to process and work through everything that had happened. God’s grace upon us was so sweet that night, His presence was so near through it all. He was and always is enough and He had undoubtedly carried us through every moment and every decision we had to take.

We can’t begin to thank our family and friends enough for holding us through this time. To those who prayed for us, we felt it – thank you! To those who fed us, thank you! To my mom for having our girls that morning and for breaking the news to them, thank you! To my mom-in-law for taking on the very emotional task of looking after our girls, talking through things with them and praying for us all, thank you. To my dad for the daily phone calls that were so full of tears, thank you. To Kath, for playing such a big role in getting us home, thank you! To my father-in-law for driving around to organise a very specific bottle for Leevi, thank you! To Karen for shopping for all the little extra’s I hadn’t packed, thank you! To Graham for being so supportive of our decision to lodge and for all the costs that it would entail, thank you! To our friends, for the messages and flowers that were sent daily, thank you!
To Dr Russouw, for taking the time to talk to me, for checking in every day to see how I was doing (despite the fact that I had been discharged days before), for really taking an interest in whether I needed the meds or not and for respecting my decision in the end, for coming to see us when we decided to transfer Leevi and for phoning every day after that until we were home, thank you!
To Dr Strachan, for being ready and waiting for us, not only with your expertise but also with a hug. For making things so simple when they had been so complicated, for helping me to bond with my boy and then for sending us home, thank you!
To our girls, for maturing beyond your years, for being so strong and so understanding, for loving your brother beyond what we ever thought was possible, for visiting and bringing pictures every single day, for being so patient and for always bringing a smile, thank you!
To Phil, my rock – for leading me, for being strong for me, for crying with me, for loving me, for praying with me and for me, for being the most amazing Dad to our girls and for holding it all together at home, for seeking and trusting God every single day, THANK YOU!























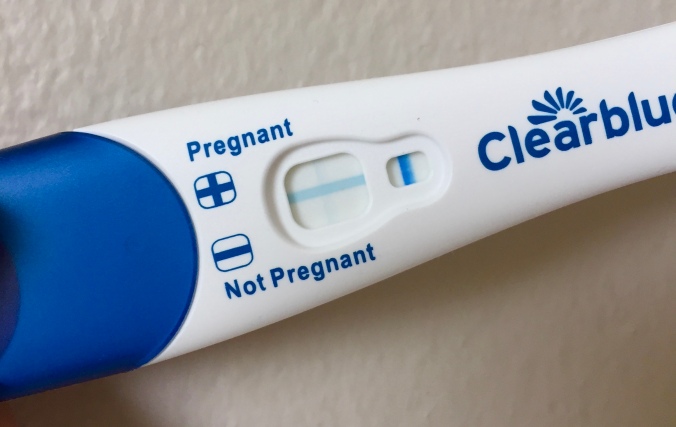
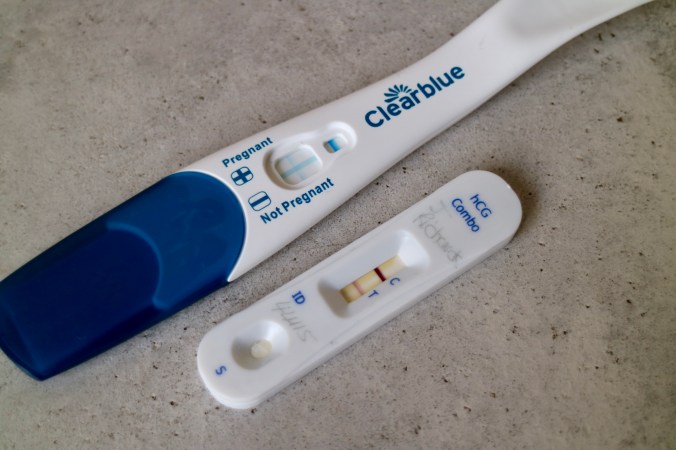
 I am still pretty much living off of strawberries, not so much peanut butter anymore and my appetite is much to be desired. I am nauseous a lot of the day and I have gone completely off meat (dinners are a challenge). I am loving cereal (particularly cooked oats) and I am thirsty ALL THE TIME. Other strange symptoms include watery eyes, which is something I haven’t struggled with in past pregnancies and amazing skin – with the girls I broke out all the time. This time, my skin has been even and soft… so it’s not all bad.
I am still pretty much living off of strawberries, not so much peanut butter anymore and my appetite is much to be desired. I am nauseous a lot of the day and I have gone completely off meat (dinners are a challenge). I am loving cereal (particularly cooked oats) and I am thirsty ALL THE TIME. Other strange symptoms include watery eyes, which is something I haven’t struggled with in past pregnancies and amazing skin – with the girls I broke out all the time. This time, my skin has been even and soft… so it’s not all bad.